Mastering the Art of Case Presentation at Conferences: A Guide for Optometrists
Presenting a case at a conference or scientific session is a great opportunity for optometrists to showcase their clinical expertise, share unique patient cases, and contribute to the broader field of eye care.
Presenting a case at a conference or scientific session is a great opportunity for optometrists to showcase their clinical expertise, share unique patient cases, and contribute to the broader field of eye care. However, delivering an effective case presentation requires careful preparation, structured documentation, and a clear, engaging delivery. This guide will walk you through how to craft and present a compelling optometry case study that resonates with your audience.
Why Case Presentations Matter
Case presentations serve multiple purposes in clinical and academic optometry:
- Educational Value: They provide insights into rare, challenging, or unique cases that can help other practitioners in their diagnosis and management.
- Professional Recognition: Presenting at a conference positions you as a knowledgeable clinician and can enhance your professional credibility.
- Networking Opportunities: Sharing your expertise can open doors to collaborations, discussions, and potential research endeavors.
- Skill Development: Preparing a case study sharpens your clinical reasoning, communication, and critical thinking skills.
Choosing the Right Case to Present
Not every patient encounter is suitable for a conference presentation. Choose a case that is:
- Rare or Unusual: A unique presentation of a common condition or a rare diagnosis.
- Challenging: Cases that required innovative problem-solving, multidisciplinary collaboration, or new treatment approaches.
- Educationally Valuable: Offers a learning opportunity for other practitioners.
- Ethically Appropriate: Ensure that patient confidentiality is maintained and that consent is obtained when necessary.
Structuring Your Case Presentation
A well-structured case presentation follows a logical flow, allowing the audience to easily follow your thought process and key findings.
1. Title and Introduction
Choose a concise, engaging title that reflects the essence of your case. Example:
- "Atypical Presentation of Keratoconus in a Young Patient: Diagnostic Challenges and Management"
- Provide a brief introduction on why this case is important and how it contributes to clinical practice.
- Highlight the key learning objectives for the audience.
2. Patient Demographics and History
- Age, gender, and relevant personal/medical history (without revealing identifiable information).
- Chief complaint: What brought the patient in?
- Onset and duration of symptoms.
- Relevant systemic or ocular history.
- Family history (especially for genetic or hereditary conditions).
- Social and occupational history if relevant.
Example:
A 22-year-old male presented with progressive blurry vision in both eyes for the past 12 months. He reported increased glare at night and difficulty with contact lenses. Systemic history of chronic hayfever since childhood, with symptoms of severe itchiness to the eyes.
3. Clinical Examination Findings
- Visual Acuity (VA): Distance and near, with and without correction.
- Refraction: Subjective and objective findings.
- Slit-lamp Examination: Any abnormalities in the cornea, lens, anterior chamber, etc.
- Fundus Examination: Key posterior segment findings.
- Special Tests (if applicable): Corneal topography, OCT, fluorescein staining, etc. It is always better to include as many images as possible for a stronger case presentation
Example:
- Unaided VA: OD 6/24, OS 6/18; best-corrected VA: OD 6/12, OS 6/9.
- Retinoscopy: OD -6.00 DS / OS -5.50 DS.
- Slit-lamp Examination: Mild corneal thinning in both eyes with prominent Vogt’s striae.
- Topography: Inferior steepening and asymmetric bowtie pattern consistent with keratoconus.
4. Differential Diagnosis
- Provide a list of possible diagnoses considered and how they were ruled out.
- Discuss why the final diagnosis was made.
Example:
Differential diagnoses included keratoconus, pellucid marginal degeneration, and post-LASIK ectasia. Corneal topography confirmed asymmetric steepening typical of keratoconus, ruling out the other conditions.
5. Management Plan and Treatment
- Discuss the treatment approach taken and justify your decisions.
- Include medical, optical, or surgical interventions (e.g., specialty contact lenses, cross-linking, etc.).
- If applicable, discuss patient education and compliance strategies.
Example:
The patient was initially fitted with corneal rigid gas-permeable lenses to improve visual acuity. Due to intolerance, scleral lenses were prescribed, achieving VA of 6/7.5 in both eyes. Corneal cross-linking was discussed and scheduled to prevent further progression.
6. Follow-up and Outcomes
- Share post-treatment results and whether the case was successfully managed.
- Discuss any complications or unexpected outcomes.
Example:
At the three-month follow-up, the patient reported improved vision and comfort. Topographic maps showed stabilization in corneal curvature. He adapted well to scleral lenses and reported minimal visual distortion.
7. Discussion and Clinical Pearls
- Summarize the key takeaways from the case.
- Relate the case to existing literature, guidelines, or best practices.
- Discuss what makes the case unique and what other optometrists can learn from it.
- If applicable, suggest areas for further research or investigation.
Example:
This case highlights the importance of early detection and intervention in keratoconus. Practitioners should consider corneal topography in young patients with unexplained astigmatism to rule out early keratoconus. Scleral lenses offer an excellent alternative for patients with RGP intolerance.
8. Conclusion
- Reinforce the main takeaways in a concise manner.
- End with a call to action, encouraging further discussion or research.
Example:
Early detection and personalized management of keratoconus can significantly improve patient outcomes. Optometrists should remain vigilant in identifying subtle signs and educating patients on available treatment options.
9. References and Acknowledgments
- Cite relevant studies, books, or guidelines referenced in your discussion.
- Acknowledge any mentors, colleagues, or institutions that contributed to the case.
Presentation Tips for Conferences
A well-documented case is only effective if presented clearly and engagingly. Here are some practical tips:
1. Keep It Structured
- Stick to the logical case flow to maintain clarity.
- Avoid excessive details that don’t contribute to key learning points.
2. Use Visuals Effectively
- Include high-quality images, charts, and videos where applicable.
- Use bullet points rather than large text blocks on slides.
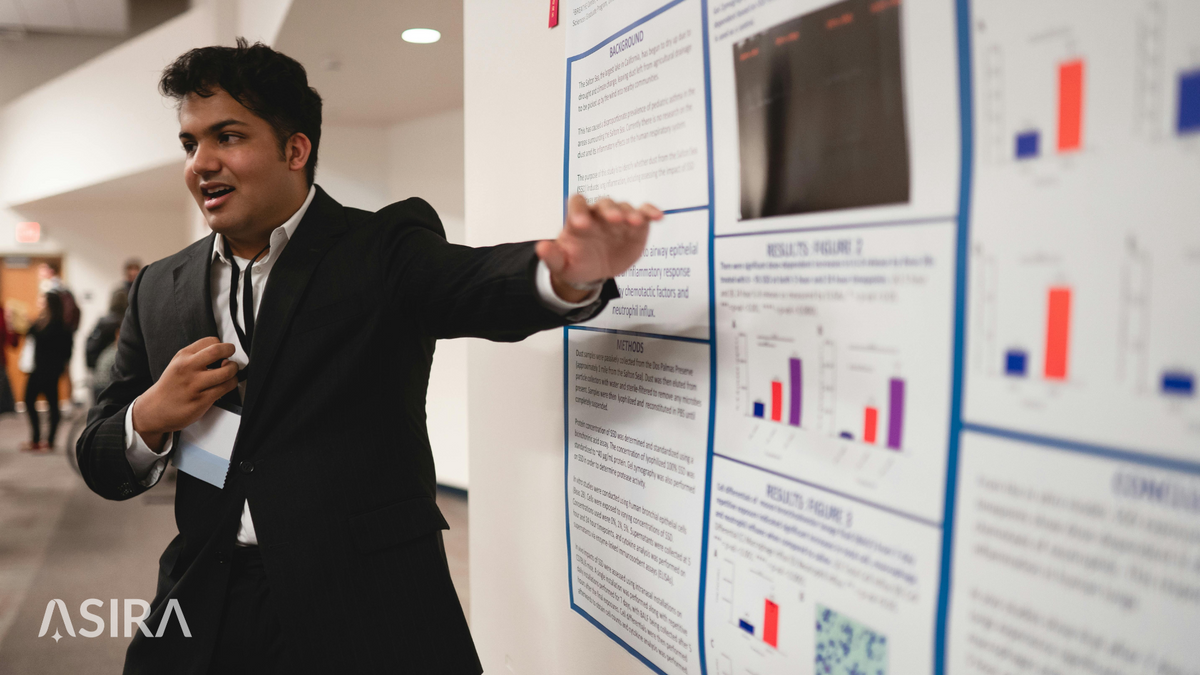
3. Engage Your Audience
- Ask rhetorical questions or pose clinical dilemmas to keep listeners involved.
- Maintain eye contact and speak confidently.
4. Time Management
- Most conferences have strict time limits; rehearse to stay within your allotted time.
- Prioritize essential information and avoid unnecessary elaboration.
5. Anticipate Questions
- Be prepared to answer questions about alternative diagnoses, treatment choices, or literature references.
- If unsure, acknowledge the question and offer to follow up.
Final Thoughts
A well-prepared case presentation can leave a lasting impression and contribute meaningfully to the optometry field. By carefully documenting your case, structuring your content effectively, and presenting confidently, you can ensure your insights are valuable and engaging to your peers.
Would you like to practice your presentation with a peer before your next conference? Consider joining an optometry discussion group or seeking feedback from mentors. Happy presenting!
ASIRA is a simple and secure, cloud-based software tool, built BY optometrists FOR optometrists, that helps eye care professionals reduce the time and effort required to maintain clinical records, schedule appointments, generate bills, manage inventory and much more!
To find out more, visit www.asira.health and sign up for a 30-Day FREE TRIAL! If you're a new practice owner or a fresh graduate thinking of entrepreneurship, visit www.asira.health/optompreneur to learn how ASIRA can help reduce your costs and increase revenue.

